Greece is “urging” citizens to get vaccinated against COVID-19, Spain has reintroduced mask-mandates inside medical establishments, American universities are still saying get vaccinated to “avoid spreading it to someone who could get seriously ill”.
COVID-19 was somewhat of a global response. Many countries followed their path, or their own interpretation of the WHO recommendations, or their own past experiences with infectious disease control. However, when taken together, the policies were largely the same.
Now, these policies from the COVID-era come with no excuse about having limited data or working in emergency situations and cramped hospitals. They come, so to speak, in the cold light of day, with many new facts, new studies, new confessions, and new realities.
On January 9th, Euro News reported that Spain’s Minister of Health, Monica Garcia, announced the return to masking mandates by calling the measure “an effective, common-sense rule that is supported by scientific evidence and well-received by the general public”.
In the fog of war that was February—June of 2020, that statement may have been acceptable, but multiple scientific institutes have put surgical masks, and even the hailed FFP2/N95 models to the test and found there’s nothing to support the idea they protect individuals from viruses.
The Cochrane Collaboration found that neither cloth, nor surgical, nor even N95/P2 masks showed any effectiveness at preventing a variety of viruses in over 600,000 people across 11 randomized controlled trials. Previously, observational evidence suggested that mask-wearing could prevent viral transmission when looked at on a population-wide level, but when subjected to the “gold-standard” of randomized controlled trials, they absolutely did not.
Among the countries surveyed were England, Norway, Bangladesh, Mexico, and Denmark. Four studies were conducted during the 2020 period of the COVID-19 pandemic, while several others were conducted during the 2009 H1N1 influenza pandemic, and others in epidemic influenza seasons up to 2016.
The settings included suburban schools and hospital wards in high‐income countries; crowded inner-city settings in low‐income countries; and an immigrant neighborhood in a high‐income country. One study included a case group of healthcare workers trained to use masks correctly for long periods.
In Spain, the mask mandate was reintroduced alongside flu case numbers, meaning the decision involved the seasonal flu in addition to COVID-19.

Social distancing: myth — Lab leak: not a myth
Some during the pandemic, for example Sweden which was famously restrained in their application of quarantine and lockdown measures, suggested that more importantly than mask wearing was social distancing, or maintaining a two-meter (6-foot) distance between yourself and others.
In a recent closed-door Congressional testimony, former head of the COVID response task force under Trump and Biden, Dr. Anthony Fauci, admitted that social distancing guidelines “just sort of appeared” and that no scientific evidence as to its effectiveness ever existed. Having admitted that, one can therefore infer that every time Dr. Fauci, or someone from the NIH or the CDC, recommended them in an official capacity, they were either knowingly lying, or were simply disgracefully negligent.
Dr. Fauci also acknowledged that the lab leak hypothesis is not a conspiracy theory despite openly dismissing it as one. This comes nearly four years after prompting the publication of the now infamous “Proximal Origin” paper that attempted to vilify and disprove the lab leak hypothesis.
The circumstantial evidence of a lab leak origin is substantial, as were the attempts to smear it and anyone open to considering it by scientific media.
Pushing vaccines
The whole point and function of living in a democracy is to be able to give people significant personal agency in an environment where they can utilize it for the benefit of themselves and their fellow man. Among that agency has to be the level of acceptable risk, which can be seen in action every day from smoking and driving cars.
If in January 2024, someone has decided to remain unvaccinated against COVID-19, one simply cannot deny that person has made a decision on the level of acceptable risk of hospitalization, or even death, and determined they can accept it.
This may be because the virus has mutated into a much less lethal form over the time it has been observed. One survey of 50 countries found that the case fatality ratio for the Omicron variant, which was present when much of the West ended all restrictions on travel and social life, was as low as 0.02 per 100,000 people, a risk of death that is simply too low to rationally understand, as it lies among the millions.
Nevertheless, countries are urging their citizens to get vaccinated. Greece opted against mandating masks and other measures, but strongly urged their citizens to wear them and get vaccinated. Today, vaccination doesn’t mean what it meant in the winter of 2021, but rather entails getting the latest dose much like seasonal influenza. Media reports total the current number of patients hospitalized from COVID-19 in the country of 10 million people at 90. The same reports say 1,000 people have died in Greece since September “linked” to COVID-19, but as was discovered time and time again during the pandemic, that rarely meant the cause of death was COVID.
A Professor of public health at Virginia Tech, Lisa Lee, has been answering questions for a media advisory on vaccination for COVID-19, and signed her reputation as a person with decades of experience in public health onto the idea of a ‘tripledemic’ of respiratory infections from flu, COVID-19, and RSV.
“Yes,” she said in response to the question of whether someone who’s already had COVID and barely noticed it should get vaccinated. “Even if you do not get very ill from having a respiratory infection, a vaccine can help you avoid getting it at all and help you avoid spreading it to someone who could get seriously ill. Vaccines work at both the individual and group levels by reducing the number of circulating cases. Less viruses floating around means fewer other people will get sick, which is important to the most vulnerable in our communities—newborns, older adults, and people with other medical conditions”.
Healthy newborns have never been at elevated risk for COVID in any of its iterations. As for the other motivations, it’s enough to say their merits, upon looking back at the COVID-19 story, remain suspect.
There is another side to this answer, which is that considering the incredibly small risk of death or hospitalization from COVID-19 in its current form, is that worth the not 0% chance of suffering from the now-well-documented heart complications that can arise from these vaccines? Whether that risk is as low as injury from COVID or higher remains debated, but it’s accepted a risk exists there.

Vitamin D and overlooked recommendations
What’s distinctly lacking from any of these “public health” advisories is any recommendation for supplementation of vitamin D, getting sunlight, or the importance of exercise even in the cold.
In one incredibly important study, researchers from Israel looked at medical data of vitamin D levels in infected individuals from the time they were infected and backward 2 years. 284 patients were looked at who caught the virus between 2020 and 2021, and those in the deficient category (with D levels <20 ng/mL) made up 87% of severe Covid-19 cases.
There are all kinds of numbers for how much and in what conditions various COVID jabs reduced the risk of hospitalization and death, but rarely do they reach 87%, such as in this post-pandemic vaccine effectiveness meta-analysis where the best single study found 73% effectiveness.
It’s not a perfect comparison, since that’s not what the 87% directly tells us, which is to say that abundant vitamin D levels were not found to reduce risk of severe COVID-19 cases by 87%, only that 87% of people who did have severe COVID-19 cases were deficient in vitamin D. But what is a perfect comparison is how much media coverage and public health advocacy messaging touches on the effectiveness of vitamin D vis-a-vis the vaccine. There’s no comparison—no health body is remarking on the former with greater frequency than the latter.
Exercise has been similarly underrepresented. One study found the standard metric for exercise, 150 minutes of moderate to intense movements per week, confers a 60% mean chance of avoiding a serious COVID outcome. The study found that even among people at risk of death for COVID-19, people with good physical activity levels were in the 19th percentile for death risk, a full two thirds less than their at-risk peers.
Case and point is this WHO statement released today praising the vaccines for reducing death rates by 54%, or 1.4 million people which isn’t very high among vaccine standards, and which is dwarfed by the number of people who died in Europe from COVID-19, which is over 2.4 million. It is absolutely reasonable to propose that strong messaging on the importance of vitamin D and exercise could have averaged a reduction in the death rate at least as good as 54% if not better.
There are no excuses for ignoring this evidence, and resuming without so much as an acknowledgement, previous policies that were defended from criticism as being implemented in good faith in conditions with limited evidence, but which can now no longer be so. WaL
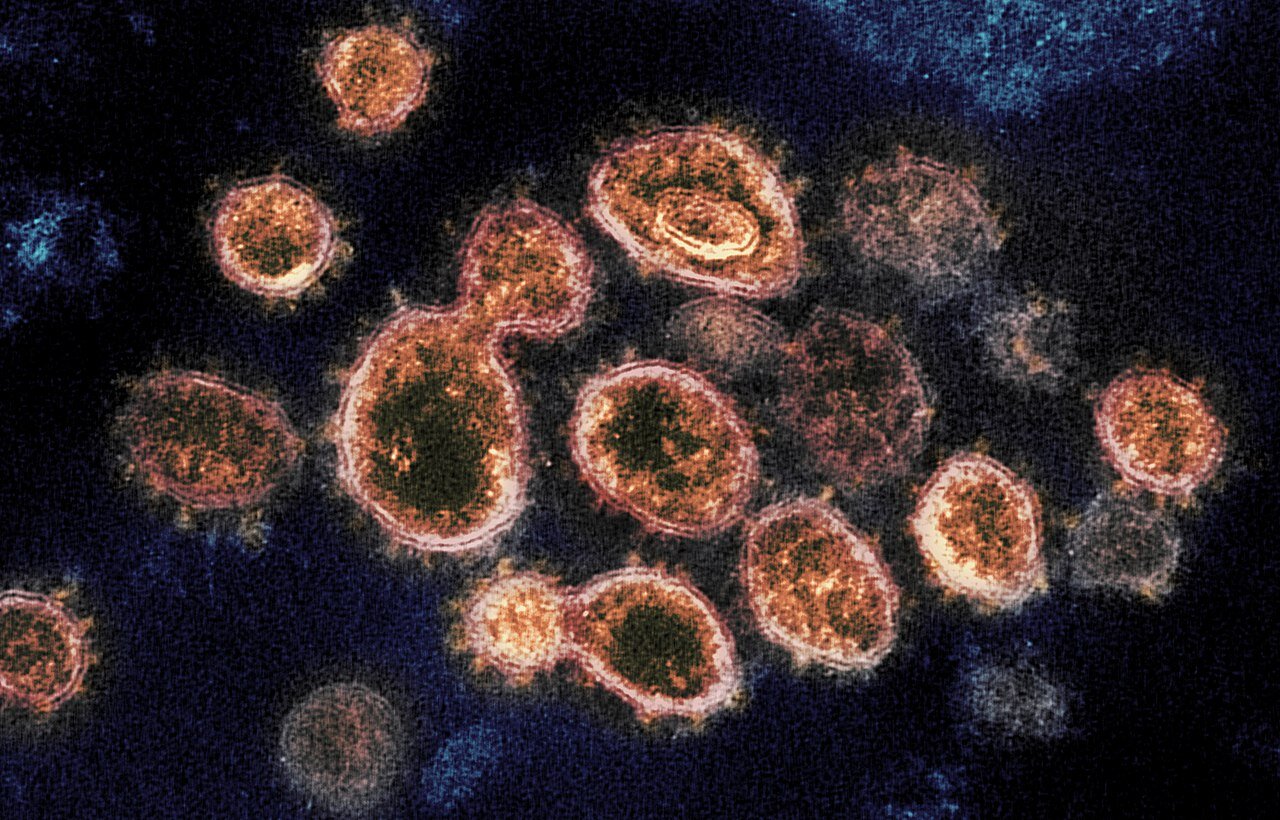
PICTURED ABOVE: The novel coronavirus SARS-CoV-2 (COVID-19). PC: NIAID. CC 2.0